Understanding Semen Quality, Sperm Lifespan, and Fertility
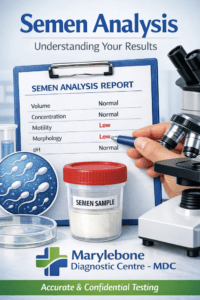
Semen analysis is one of the most informative assessments in reproductive medicine.
It provides clear insight into sperm production, function, and overall fertility potential.
At Marylebone Diagnostic Centre, 73 Baker Street, all laboratory testing is performed with a focus on accurate measurement, careful interpretation, and data-driven reporting to support confident clinical decision-making.
Semen Quality
Semen quality refers to the collective characteristics of the ejaculate, including sperm count, motility, morphology, and volume. These parameters indicate how effectively sperm can fertilise an egg.
Core Parameters:
- Volume: Typically ranges between 1.5–6.0 mL per ejaculate. Low volume may indicate obstruction, incomplete collection, or ejaculatory dysfunction.
- Sperm Concentration: The number of sperm cells per millilitre of semen. The World Health Organization (WHO, 2021) defines normal concentration as ≥15 million/mL.
- Motility: The proportion of sperm showing active movement. Progressive motility above 40% is considered favourable for fertilisation.
- Morphology: The percentage of sperm with normal head, midpiece, and tail structures. Morphologically normal sperm are better suited for oocyte penetration.
- Vitality and pH: Assessed to determine overall sperm health and seminal plasma environment.
Semen quality is influenced by factors such as temperature exposure, hormonal balance, nutrition, alcohol intake, and oxidative stress.
How Long Does Sperm Live?
The lifespan of sperm depends on the environment in which it exists.
- Outside the body: Once exposed to air and drying, sperm cells die within minutes.
- Inside the female reproductive tract: Sperm can survive for up to 3–5 days in optimal cervical mucus and reproductive conditions.
- In laboratory storage: Sperm preserved by cryogenic freezing can remain viable for many years if maintained under correct conditions.
Sperm longevity within the body is vital for conception, as ovulation timing varies. Fertile cervical mucus plays a key role in sustaining sperm viability during this period.
How Long Does Sperm Last in the Male Body?
Sperm cells are produced continuously in the seminiferous tubules of the testes through a process called spermatogenesis.
This process takes approximately 64–74 days from stem cell to mature spermatozoon. Mature sperm are stored in the epididymis, where they can remain viable for several weeks before being reabsorbed or expelled.
Healthy spermatogenesis relies on adequate testosterone levels, balanced temperature within the scrotum, and intact testicular tissue structure.
What Is a Sperm Cell?
A sperm cell (spermatozoon) is the male reproductive cell responsible for delivering genetic material to the egg during fertilisation.
Each sperm cell has three main structural components, each with a specific function.
Head:
Contains the nucleus with 23 chromosomes, along with the acrosome, which holds enzymes required to penetrate the egg.
Midpiece:
Rich in mitochondria, providing the energy needed for sperm movement and function.
Tail (flagellum):
Enables motility, allowing the sperm to swim through cervical mucus and progress towards the egg.
The structure and function of each part are critical.
Abnormalities in shape, energy production, or movement may reduce fertility or impair successful fertilisation.
DNA Fragmentation
Sperm DNA fragmentation refers to breaks or damage within the genetic material of sperm cells.
Even when routine semen parameters appear normal, elevated DNA fragmentation can affect fertility outcomes, embryo quality, and pregnancy success rates.
Common Causes:
- Oxidative stress (from smoking, pollution, or infection)
- Febrile illness or prolonged heat exposure
- Varicocele (dilated scrotal veins)
- Age-related genetic instability
Testing and Interpretation
The DNA fragmentation index (DFI) is measured through specialised assays such as SCD (Sperm Chromatin Dispersion) or TUNEL tests.
A DFI of <15% is generally considered normal, while values >30% suggest a higher risk of infertility or recurrent pregnancy loss.
Treatment focuses on identifying and managing contributing factors, often through lifestyle optimisation or antioxidant therapy.
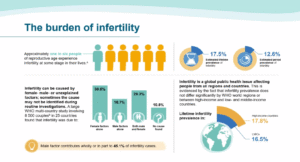
Fertility and Semen Health
Male fertility depends on the combined performance of several systems – hormonal balance, sperm production, sperm quality, and DNA integrity.
A comprehensive fertility evaluation includes:
- Semen analysis (count, motility, morphology, vitality)
- DNA fragmentation testing
- Hormonal profile (FSH, LH, testosterone, prolactin, SHBG)
- Infection or oxidative stress markers
When abnormalities are identified, clinicians can recommend evidence-based interventions ranging from nutritional support and hormonal regulation to assisted reproductive techniques.
Summary
| Parameter | What It Indicates | Typical Range/Insight |
| Semen Quality | Overall sperm health and function | Normal concentration ≥15 million/mL |
| Sperm Lifespan (Female Tract) | Fertile window post-intercourse | Up to 5 days |
| Sperm Lifespan (Male Body) | Storage before ejaculation | Several weeks |
| DNA Fragmentation | Integrity of genetic material | <15% preferred |
| Fertility Assessment | Reproductive potential | Combination of semen, hormonal, and genetic testing |
Scientific Insight at Marylebone Diagnostic Centre
At Marylebone Diagnostic Centre, semen analysis and DNA fragmentation testing are performed according to the Marylebone High Standard, ensuring precision and confidentiality.
Advanced laboratory assessments help clinicians interpret fertility potential and support evidence-based decision-making for both natural and assisted conception pathways.
Read More
- World Health Organization – Laboratory manual for the examination of human semen (6th edition)
- NHS – Semen analysis test
- Mayo Clinic – Male infertility
- Human Fertilisation and Embryology Authority (HFEA) – Sperm testing and fertility treatment
- National Institute for Health and Care Excellence (NICE) – Fertility problems: assessment and treatment