Low Sperm Count – Causes, Signs, and How to Improve It
Low sperm count is one of the most common male fertility issues. Yet, it’s also one of the most misunderstood. Many men don’t realise how common it is or that it’s often reversible.
At Marylebone Diagnostic Centre (MDC), we help men understand and improve their fertility through accurate testing and tailored guidance. Our clinic in 73 Baker Street, London, offers discreet, same-day semen analysis and full fertility profiling.
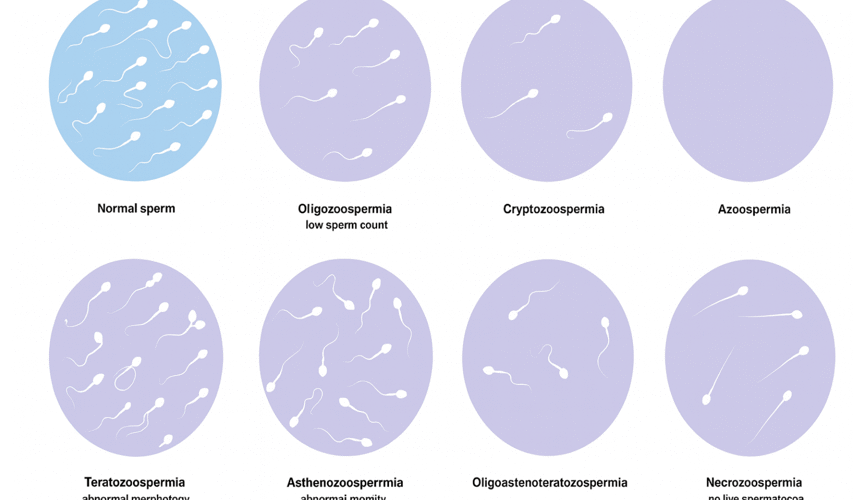
What does “low sperm count” actually mean?
A low sperm count, or oligospermia, means your semen contains fewer sperm than the typical healthy range. The World Health Organization (WHO) defines normal sperm concentration as 15 million sperm per millilitre or more.
Counts below this level can make conception harder, though not impossible. Fertility depends on more than numbers – movement, shape, and DNA quality also play roles.
Why it matters
Sperm cells carry half of the genetic material needed to create new life. If the count is low, fewer sperm reach the egg. Even if one succeeds, sperm with poor structure or movement may struggle to fertilise.
Knowing your sperm count helps identify whether the cause of infertility lies with the man, the woman, or both. It allows targeted, efficient treatment – avoiding months of guesswork.
Common causes of low sperm count
Many factors can influence sperm production. Some are temporary and lifestyle-related; others involve medical conditions.
1. Hormonal imbalance
The pituitary gland and testes regulate testosterone and sperm production. If this balance changes, sperm output can drop.
2. Varicocele
Enlarged veins in the scrotum can increase local temperature and impair sperm formation. It’s a common, treatable cause of low count.
3. Infections
Certain infections, such as sexually transmitted infections, mumps, or prostatitis, can block or damage sperm pathways.
4. Medication and substances
Anabolic steroids, chemotherapy, and certain antidepressants can temporarily or permanently reduce sperm production.
5. Heat and tight clothing
Frequent sauna use, laptops on the lap, or tight underwear can raise testicular temperature, reducing sperm health.
6. Lifestyle habits
Smoking, alcohol, stress, obesity, and poor diet all lower testosterone and sperm quality.
7. Environmental factors
Exposure to pesticides, plastics, and heavy metals may also interfere with sperm formation.
Signs of low sperm count
Most men with low sperm count have no obvious symptoms until they start trying for a child. However, some signs can indicate underlying issues:
- Difficulty conceiving after six months of unprotected intercourse
- Reduced sexual drive or performance
- Testicular pain or swelling
- Reduced body or facial hair (a sign of hormone imbalance)
- Small or soft testicles
If any of these apply, early testing is advised.
Testing for low sperm count at Marylebone Diagnostic Centre
Our Semen Analysis test is the first step. It measures:
- Sperm count and concentration
- Motility – how well sperm move
- Morphology – sperm shape and structure
- Volume and pH of the semen
The test is simple and confidential. You provide a sample in a private room or at home using secure collection kits. Results are typically ready within 24–48 hours.
Profile options
Semen Analysis – £179
Basic fertility screen measuring count, motility, and morphology.
Comprehensive Fertility Profile – £545
Includes semen analysis, hormonal blood tests (FSH, LH, Testosterone, SHBG, Prolactin, Albumin, PSA), and sperm photographs.
Advanced Care Profile – £932
Includes DNA fragmentation, hormone testing, mineral hair analysis, and semen analysis – ideal for couples trying for over 12 months or after IVF failure.
These profiles give a detailed overview of male fertility and can detect deeper issues beyond sperm numbers.
What your results mean
Your report includes several values. Understanding them helps guide next steps.
| Parameter | Typical Reference Range |
| Sperm Concentration | ≥15 million/ml |
| Total Count | ≥39 million per ejaculate |
| Total Motility | ≥40% |
| Progressive Motility | ≥32% |
| Morphology | ≥4% normal forms |
If results are outside these ranges, your clinician will discuss possible causes and treatment paths.
Can low sperm count improve naturally?
Yes. In many cases, sperm count improves with small lifestyle adjustments. The body produces new sperm roughly every 70-90 days, so positive changes show in three months.
Lifestyle actions that help
- Quit smoking and reduce alcohol – both damage sperm DNA.
- Maintain healthy weight – excess body fat lowers testosterone.
- Exercise moderately – boosts circulation and hormone balance.
- Eat nutrient-rich foods – zinc, folate, vitamin C, and omega-3 fats support sperm quality.
- Stay cool – avoid overheating from saunas or tight trousers.
- Sleep well – proper rest supports testosterone production.
- Manage stress – mindfulness or relaxation therapy can improve hormonal balance.
At Marylebone Diagnostic Centre, our clinicians can recommend tailored nutritional or lifestyle plans based on your test results.
Medical treatment options
If lifestyle changes aren’t enough, several medical solutions exist:
- Hormone therapy – corrects low testosterone or pituitary imbalance.
- Surgery – fixes varicoceles or blocked ducts.
- Medication – treats infection or inflammation in the reproductive tract.
- Assisted reproduction – IVF or ICSI may bypass sperm count barriers.
Your clinician will guide you through options suited to your individual profile.
How stress affects sperm count
Stress releases cortisol, which suppresses testosterone production. Over time, this affects sperm quantity and quality.
Regular physical activity, relaxation techniques, and sufficient sleep can help restore balance.
Can supplements help?
Certain supplements may improve sperm quality, but evidence varies. Ingredients like zinc, selenium, L-carnitine, and coenzyme Q10 show some benefit.
Always seek advice before starting supplements – self-medication can sometimes do more harm than good.
Sperm count and age
Sperm production declines slowly with age. From around age 40, motility and DNA integrity may decrease.
That’s why early testing, even if you’re not trying to conceive yet, can provide valuable baseline data.
FAQs
Why choose Marylebone Diagnostic Centre
- Central London location near Baker Street Station
- Discreet, professional testing environment
- Fast, reliable results analysed by biomedical scientists
- Packages tailored to your fertility stage
- Guided consultations and ongoing care
Our goal is to make male fertility testing simple, accurate, and approachable.
Take the next step
If you’re concerned about fertility, don’t wait. A simple test can reveal valuable information about your reproductive health.
Book your Semen Analysis or Comprehensive Fertility Profile today at Marylebone Diagnostic Centre, 73 Baker Street, London W1.
Call +44 7495 970109 or visit marylebonediagnosticcentre.com.
Understanding your sperm count is the first step toward improving it – and your future family’s journey.